FDA approves new drug; may help stop rare/fatal condition doctors call ‘ticking time bomb’
Brenda Goodman, CNN | 3/27/2024, 12:51 p.m.
When doctors told Katrina Barry that she had a rare and serious condition called pulmonary arterial hypertension or PAH, they warned her not to Google it.
Come on, she thought; they wanted a young woman who was bound for graduate school, who had survived a transatlantic plane flight while having a heart attack and now open-heart surgery, not to look up the condition that kept trying to kill her?
Waiting for her on the internet was some chilling information. PAH affects about 500 to 1,000 Americans each year, often women between the ages of 30 and 60, according to the American Lung Association.
Barry, who was 25 at the time, learned from her reading that she had two to five years to live, based on how severe her condition already was.
Then her medical team offered her a potential lifeline: a first-of-its-kind experimental drug called sotatercept that corrals a growth factor that is overproduced by people with PAH, potentially changing the underlying biology of the disease.
She signed up for a study to test the medication, given every three weeks by injection under the skin.
She started treatment at the dawn of the Covid-19 pandemic, in March 2020. Barry said she diligently wore an N95 mask and two layers of clothing and scrubbed herself down after every trip to the hospital for her injections to avoid getting Covid along the way.
“I had to go to the hospital because I was dying if I didn’t get this drug,” she said. “This was the only chance I had at survival.”
On Tuesday, the US Food and Drug Administration approved the medication that Barry has taken for four years, a drug she credits with keeping her alive and allowing her to resume many of the activities she enjoyed before her diagnosis.
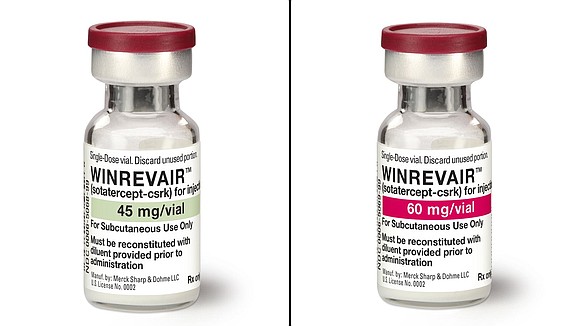
Merck, the company that manufactures the drug, said it will be sold under the brand name Winrevair.
Barry, now 29, is a patient consultant for Merck but said she has not received compensation for telling her story.
Winrevair is a biologic drug designed to grab onto and trap proteins called activins that are overproduced in PAH. These proteins cause the walls of a person’s blood vessels to keep growing and thicken over time.
As the blood vessels narrow, the heart is forced to work harder to pump blood to the lungs. This stress eventually damages the heart, causing it to fail.
Without treatment, people who have PAH usually live about two to three years after their diagnosis. Treatment with a combination of drugs that dilate, or relax, blood vessels can improve this outlook, but they are not a cure.
“This medication has a much different mechanism of action, and it may actually rebalance some of the growth that goes on in … the very small pulmonary arterioles where the disease starts,” said Dr. Vallerie McLaughlin, a cardiologist at the University of Michigan who helped study sotatercept.
“That may attack the disease from a different angle and allow for what we returned as reverse remodeling,” she said, meaning patients could actually improve over time while on the medication.
Winrevair is the first new type of drug to come along for patients with PAH in a long while, said Dr. Panagis Galiatsatos, a pulmonary and critical care medicine specialist at Johns Hopkins Bayview Medical Center and a spokesperson for the American Lung Association.
In animal studies conducted before the human trials, the drug looked like it could do more than just treat symptoms: It seemed like it might be able to stop the thickening of the blood vessels and perhaps prolong patients’ lives, but those benefits have not been proven in humans.
Instead, Galiatsatos said, the FDA approved the drug based on other signs of effectiveness, including whether patients were able to walk farther in six minutes than they could before they started taking the drug, a clinical measure called the six-minute walk test.
In a study that included 323 people who took either sotatercept or a placebo for six months, those who got the drug were able to walk 34 meters – about half a city block – farther in six minutes than they could before they started treatment, while people in the placebo group were about to walk only about 1 meter more than they could when they started the study. Both groups were also taking the standard medications for the condition, which help relax blood vessels to improve blood flow.
By the end of the study, nine participants, or about 5%, in the sotatercept group had died or had their disease worsen, while 42 patients, or about 26%, in the group taking a placebo had died or gotten worse.
The FDA was willing to act fast to approve the medication because the disease, Galiatsatos said, is a “ticking time bomb” for people who don’t have time to wait for longer studies.
The study that led to the drug’s approval was published in the New England Journal of Medicine last year.
“Many of us are excited about a medication such as this, so we can offer our patients something that we believe is better than their current standard of therapy,” said Galiatsatos, who noted that neither he nor the American Lung Association has any financial interest in the drug.
But Galiatsatos said that as promising as the drug looks, there are still many unknowns, including whether the drug will benefit all PAH patients equally. Although a significant number of people who are diagnosed with the disease are African American, he noted, just seven people in the clinical trial – representing 2% of participants – were Black.
“I tend to hold my breath” with any new drug, Galiatsatos said, adding that he “is waiting for the real-world data to pour in to see how well this worked in more diverse patients.”
Like ‘a miracle’
In July 2019, Barry had rented an apartment for the summer in Greece, where she was looking forward to volunteering at a children’s hospital. But while she was abroad, some shortness of breath that she had been asking doctors about for more than two years suddenly worsened.
She woke up one morning gasping for air and realized the situation was dire. She knew she had to get back home to Boston for help. She called her mom, and they booked a flight for her back to the States.
She landed at the airport and went straight to the hospital. There, doctors did a CT scan and found what looked like dozens of blood clots in the tiny vessels that lace the lungs. Her heart had been severely damaged by a heart attack.
“The cardiologist said that my level of heart damage isn’t found until autopsy,” Barry said. “And every doctor said I should not have survived that plane ride home.”
A delicate operation to remove the clots followed – but the surgeons who opened her chest found that her blood vessels had actually collapsed in many areas, mimicking blood clots. The blood pressure inside her heart was sky-high, and that’s when they finally knew what they were dealing with PAH, she said.
Because the disease is rare and often affects younger women, delays in getting a diagnosis are unfortunately common, Barry said.
As doctors were warming Barry’s body to bring her out of surgery, her heart wouldn’t restart. She spent a week in an induced coma on a heart-lung bypass machine. The medical team told her parents that she would probably need an immediate heart-lung transplant.
After a few days on the bypass machine, however, her body began to recover, and doctors were able to bring her out of the coma.
When she woke up, she learned about her pulmonary hypertension diagnosis.
At 25, facing a life far shorter than expected, Barry saw everything differently.
“Why am I saving if I’m not going to have a retirement?” she wondered. “Let me enjoy the life that I have now.”
But there wasn’t even much of life left to enjoy, she said.
She was tethered to oxygen tanks and forever wondering how many she would need for the amount of time she wanted to be out of the house. There was also a large new medication pump that lived in a fanny pack she could never take off, even to shower.
The pump delivered a continuous stream of drugs through a catheter threaded directly into a large vein in her body to help keep her blood vessels open. If something ever happened to the pump, she had three hours to get to the nearest hospital for help, she was told.
Being alive was nice and all, Barry thought, but what about wearing a dress? What about going for a swim?
“The list goes on of all the things I could not do,” she said.
Barry was diagnosed shortly after her surgery in October 2019, and she jumped at the chance to try sotatercept in the spring of 2020. The improvements weren’t instant, but after a few months, she went from not being able to even fold her laundry to being able to do a little more. She was able to go for short hikes and kayak a bit.
After a year, Barry said, she was able to come off her continuous oxygen therapy and use it only at night. She was eventually able to stop using it at night, too.
After about 18 months, doctors were able to remove her central line and the bulky, ever-present med pump, allowing her to switch from the IV versions of her vasodilating drugs to the pill forms.
“For me, that was so life-changing,” Barry said.
She improved so much, she was able to go back to Greece in 2022 and hike up a volcano. Last month, she went skiing.
Barry still has PAH. Her lungs burn and she gets short of breath whether she exerts herself a lot.
“But it has gotten better over time,” Barry said.
She’s enrolled in a master’s degree program in public health, and she was able to wear a dress to her brother’s wedding. She has not needed the heart-lung transplant that doctors thought she might.
“It’s a miracle drug, honestly,” she said of sotatercept. “That sounds weird to say, but it gave so much positive but not much negative.”
She does know at least one person in the tightly knit PAH community who experienced bleeding while on the drug and had to stop taking it.
Bleeding and dizziness among the risks
In clinical trials, people on sotatercept had more nosebleeds because of burst blood vessels in their noses, and they developed more spider veins under their skin. Experts say the drug may spur the growth of new blood vessels.
Other side effects included dizziness and increased hemoglobin, the molecule that carries oxygen in the blood. Some people with PAH already have elevated hemoglobin levels as their bodies try to compensate for the condition, so adding the drug on top of that might be too much for them, experts said.
Sotatercept can also decrease platelets, the cells that help form clots, which increases the risk of bleeding.
“There’s been some reports of gastrointestinal bleeding and even bleeding within the brain,” said Dr. Kristin Highland, a lung specialist at the Cleveland Clinic who treats people with PAH. “So bleeding is probably a real side effect.”
Doctors who have tested sotatercept believe that it could be a big advance. But they also acknowledge that there are still a lot of unknowns, such as whether people on sotatercept will need to keep taking the cocktail of drugs that help to relax their blood vessels and lower their blood pressure, Highland said.
“That’s the million-dollar question,” she said. “Certainly, there’s a lot of hope that maybe this would allow lower doses or possibly one of those therapies to be removed. But I don’t think we quite have the answer to that.”
Merck says it plans to charge a wholesale cost of $14,000 per vial and dosing is based on a patient’s weight. The medication will come in single or double vial kits that can be used at home.
Based on data from clinical trials, Merck says, it expects that most patients will need a single vial every three weeks, for an annual cost of about $243,000.
The wholesale cost isn’t typically what patients pay. The final cost to individuals is determined after insurance providers negotiate the price.
Still that’s significantly more than some analysts had hoped to see. The nonprofit Institute for Clinical and Economic Review said the benefits of the drug would be worth the cost at around $35,000 per year.
Merck said in a news release that it expected the drug to be in specialty pharmacies by the end of April.
At least initially, patients have to get their injections of sotatercept in a clinic, where they can be monitored. Over time, Barry said, she was able to begin giving herself the injections at home, which has made it more convenient.
Dr. Aaron Waxman, Barry’s doctor and the director of the pulmonary vascular disease program at Brigham and Women’s Hospital in Boston, said he’s seen other patients who’ve done as well as she has in the six years they’ve been studying the drug. Those people have also been able to get off their med pumps and switch to pills for their other therapies.
One such pill – Opsynvi, a new combination of two commonly taken drugs made by Johnson & Johnson – got FDA approval on Monday to treat PAH.
“We are seeing marked improvement that would suggest reversal” of disease with sotatercept, Waxman said.
“I’ve never seen this kind of improvement in the disease before,” he said. “I think this will be a game-changer.”
Barry says the drug has already been a beacon for people who may not have much to fight for.
“It’s brought so much hope to people who who’ve lost all hope because of this fatal disease,” she said.